Your menstrual cycle is orchestrated by a sophisticated interplay of hormones that fluctuate throughout each phase. Understanding how these hormonal changes affect your body can help you better recognize what's normal, anticipate changes in mood and energy, and make informed decisions about your reproductive health.
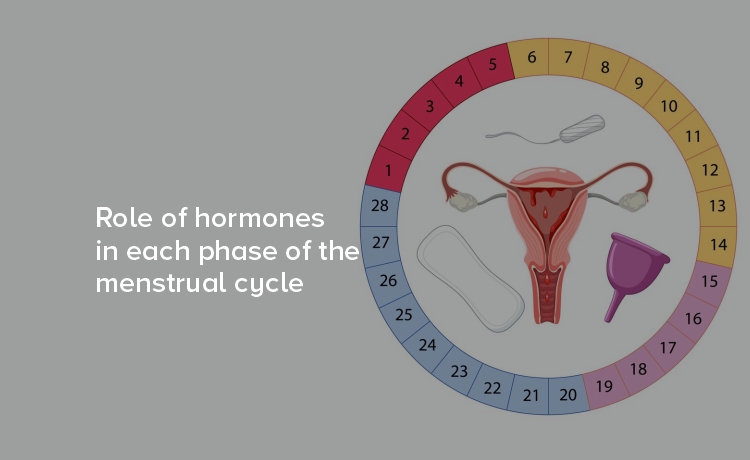
The average menstrual cycle lasts 28 days, though cycles ranging from 21 to 35 days are considered normal. Throughout this time, four key hormones—estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH)—rise and fall in precise patterns to prepare your body for potential pregnancy each month.
Your menstrual cycle consists of four distinct phases, each characterized by unique hormonal patterns that serve specific biological purposes.
The menstrual phase marks the beginning of your cycle, starting on the first day of your period. During this phase, hormone levels are at their lowest point.
This hormonal decline signals your body to release the thickened endometrium that built up during the previous cycle. Many women experience cramping during this phase as the uterus contracts to expel this tissue.
The low hormone levels during menstruation can affect energy levels and mood. You might notice decreased motivation or feel more introspective during these days, which is completely normal and reflects your body's natural rhythms.
The follicular phase overlaps with menstruation and continues until ovulation. This phase is characterized by rising estrogen levels as your body prepares to release an egg.
The hormonal fluctuations in follicular phase often correspond with improvements in mood and energy. As estrogen rises, many women report feeling more optimistic, energetic, and mentally sharp. This hormone also promotes collagen production, which can give your skin a healthy glow.
The increasing estrogen levels during this phase serve multiple purposes: they stimulate the growth of the uterine lining in preparation for potential implantation and help mature the egg that will be released during ovulation.
Ovulation represents the peak of your cycle's hormonal activity and typically occurs around day 14 of a 28-day cycle.
The LH surge is so significant that ovulation predictor kits detect this hormone to identify your most fertile days. This surge causes the mature follicle to rupture and release the egg into the fallopian tube.
During ovulation, you might notice changes in cervical mucus, which becomes clearer and more slippery due to high estrogen levels. Some women also experience mild pelvic pain called mittelschmerz, which occurs when the follicle releases the egg.
The luteal phase begins after ovulation and lasts until your next period starts. This phase is dominated by progesterone, which prepares the body for potential pregnancy.
Progesterone serves as the primary hormone during this phase, maintaining the thickened uterine lining and preparing the body for potential implantation. This hormone also raises your basal body temperature slightly, which is why fertility tracking often includes temperature monitoring.
The luteal phase can bring noticeable symptoms as hormone levels fluctuate. High progesterone may cause bloating, breast tenderness, and changes in appetite. Some women experience premenstrual syndrome (PMS) during the later part of this phase as hormone levels begin to decline.
The hormones in menstrual cycle don't just affect your reproductive system—they influence your entire body and mind throughout the month.
Understanding these patterns helps you recognize that monthly variations in how you feel are normal and hormonally driven. This knowledge empowers you to plan activities around your natural rhythms and seek support when needed.
While hormonal fluctuations are normal, certain symptoms warrant medical attention. Consider consulting a healthcare provider if you experience:
A healthcare provider can evaluate whether your symptoms indicate a hormonal imbalance or other underlying condition that may benefit from treatment.
Several lifestyle factors can help support healthy hormonal balance throughout your menstrual cycle:
Regular exercise can be particularly beneficial, though you might find your energy and performance vary throughout your cycle. Gentle activities during menstruation and more intense workouts during the follicular phase often align well with natural energy fluctuations.
Your menstrual cycle represents a remarkable example of your body's ability to regulate complex biological processes. The precise coordination of hormones in menstrual cycle demonstrates the sophisticated nature of reproductive health.
Rather than viewing monthly changes as inconveniences, consider them indicators of your body's healthy function. Each phase serves important biological purposes, and the hormonal fluctuations in follicular phase and throughout your cycle reflect your reproductive system working as designed.